EUHPP THEMATIC NETWORK ON
HEALTHCARE in
CROSS-BORDER regions
Recommendations for Policy Actions
Introduction
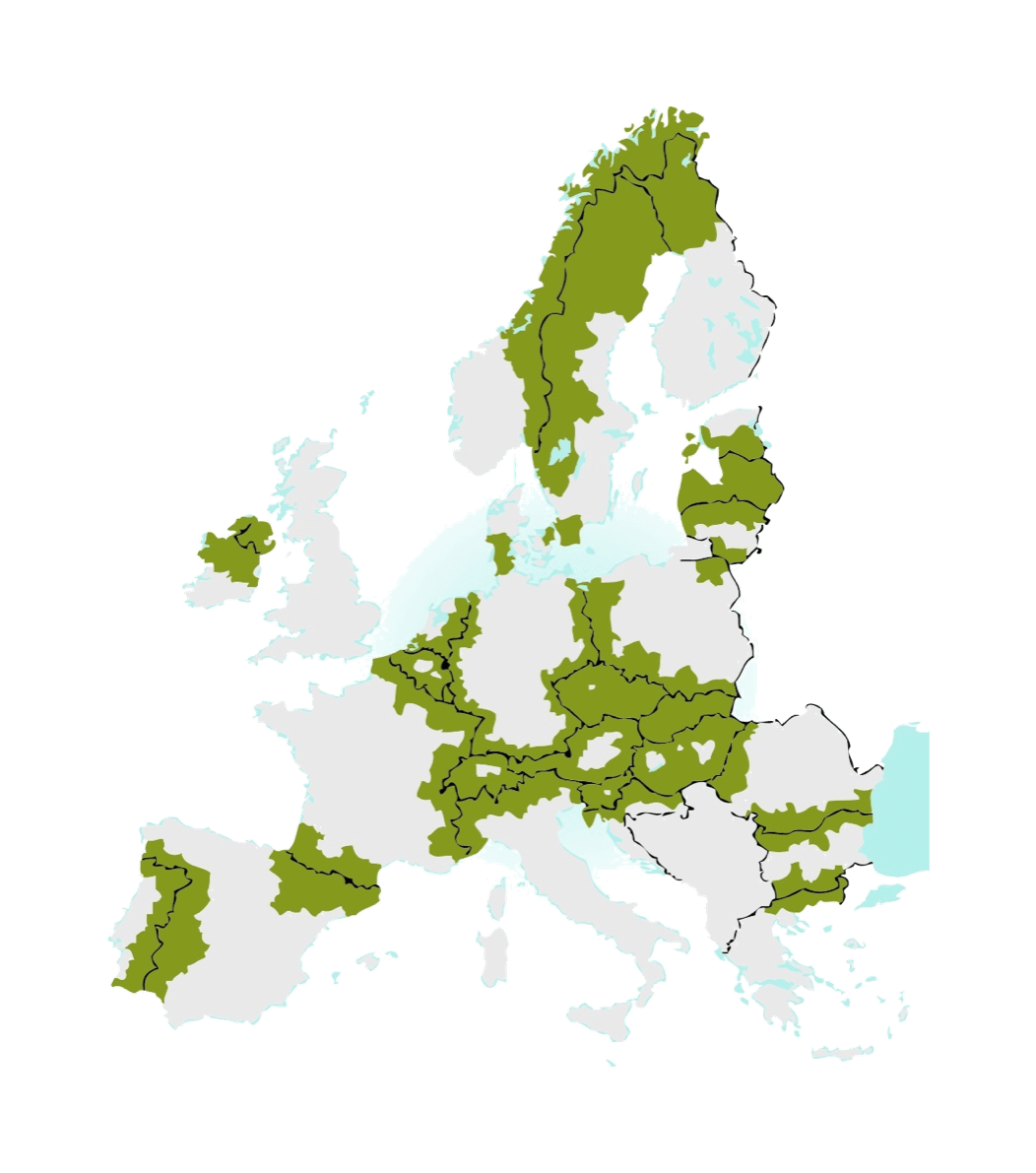
The European Union covers over 4 million km² and has 508 million citizens. Together with the immediate neighbours from the EFTA Association, it counts 40 internal land borders among the 28 Member States. Border areas are home to 30% of the European population – 150 million citizens respectively.
The socio-economic development of border regions is often hampered because of their peripheral location and the differences in legislation compared to their neighbouring countries. Border regions experience hindrance of free movement of labour and services which leads to disadvantages in the economic, social and cultural development. In addition, all these factors significantly affect healthcare systems in border regions. The geographical working area for enterprises and their markets (especially in the case of SMEs), healthcare providers and institutions, skills and training services for the workforce, educational institutions and regional governments often encounter more obstacles than in non-border regions, which makes the delivery of healthcare less efficient. Furthermore, citizens are limited in their choice of and accessibility to health care and there is less room for cooperation in the healthcare. A situation that can potentially create health inequalities.
Healthcare is a national competence and Member States finance, manage and organize their healthcare systems on their own. Nonetheless, regions and local authorities share responsibilities and competencies in the sector and the European Union supports cooperation among Member States. Therefore, sub-national authorities in collaboration with the European Commission, the European Parliament, the Member States and all the relevant health stakeholders can jointly address the challenge of delivering health and care in border areas, thus improving health for all European citizens and ensure health equity.
The Directive 2011/24/EU on patients’ rights in cross-border healthcare is an important step forward for European health policies, responding to the needs of EU citizens. The directive ensures patients’ rights to access safe and high-quality healthcare across national borders in the EU and their right to be reimbursed for such healthcare. The effectiveness of the directive varies between Member States and regions and more needs to be done to overcome some of the challenges related to documentation, reimbursement, translation and equal access, to name only a few. While a number of good practices already exists in the field of cross-border care, it shall be noted that cross-border cooperation does not include new challenges such as differences in structures and legislation, fragmented roles and various responsibilities in healthcare, and a more complex setting for health care providers and their markets.
To better address such challenges, on 20 September 2017 the European Commission adopted its Communication “Boosting Growth and Cohesion in EU Border Regions”, which highlights ways in which the EU and its Member States can tackle the issue by promoting the pooling of services along internal borders. The Communication proposes a set of actions to enhance competitiveness and cohesion in border regions, notably by addressing some of the legal and administrative barriers currently hampering closer cooperation and interaction. Moreover, the report of the Commission on the operation of Directive 2011/24/EU on the application of patients’ rights in cross-border healthcare stresses the need to map and build cross-border and regional cooperation.
With this joint statement and thematic network, it is the aim of EUREGHA and the “Healthacross initiative” of Lower Austria and all the supporting organisations, to complement the European Commission’s efforts to map crucial challenges in cross-border and regional cooperation in health care and to identify successful experiences, which could be scaled up. A participatory approach is used, and all stakeholders concerned with cross-border healthcare are welcome for ideas and comments.
Together, we want to speak with one voice, to improve the health and well-being of citizen living in border regions and to ensure equitable access to quality healthcare close to home.
This Joint Statement is not about medical tourism and harmonisation of the Member States’ health systems. This work intend to advocate for access quality healthcare closest to home in border regions.
The vision
WE ADVOCATE FOR:
- Enabling EU citizen living in border regions to access quality healthcare services closest to home, even if across national boundaries;
- Making healthcare without borders a given for all in the EU in the not-too-distant future.
- Removing obstacles and creating more equity in accessing healthcare facilities in all European territories;
- Achieving growth and positive economic effects through a functioning cross-border collaboration in healthcare.
- “Ever closer union” – tackle health inequalities within the EU and allowing health not to stop at internal borders;
- Emphasizing the role of citizen, regional and local authorities at the heart of health policy making.
 Diversity &
Diversity &
bottom-up initiatives
FOR HEALTHCARE IN CROSS-BORDER REGIONS WE CALL TO:
- understand the diversity of health needs and its impacts on health and well-being;
- keep on sharing good-practices and experiences to allow mutual learning;
- support participatory approaches in regional health policy making;
- create suitable funding opportunities within the new funding period 2021-2027 to continue and boost innovative cross-border collaboration in healthcare.
When speaking of cross-border healthcare one must be aware, that border regions offer incredible diversity. The realities of one border area will not match the realities in any other. Therefore, any recommendation for or change in healthcare in cross-border regions must be customized for the prevailing conditions. It is not feasible to find a “one-size-fits-all” solution.
The diversity can be seen in various factors, such as geographical conditions, historic development, culture and languages. On top, every health system is organised differently. A great variety of stakeholders (i.a. civil society, interest groups, healthcare professionals, regional and local authorities, governments, insurance and industry) and their miscellaneous importance as well as different habits of the user, the (potential) patient, shape the healthcare sector and with it, any ongoing change process.
When looking at the healthcare sector one must also bear in mind the part one is looking at. Often, the focus is too narrowly put on the hospital and primary care sector. Public health in all its facets is left behind. Still, also prevention and promotion should not stop at internal borders and within country specific legislation. We thereby stress the importance of local and regional bottom-up initiatives, which create tailor-made improvements in border regions that can, sometimes more sometimes less, be adopted in other cross-border regions. Such initiatives are often initiated by citizens, civil society, interest groups or regional and local authorities, since they are confronted with cross-border issues every day and naturally seek for improvements. Participatory approaches thereby play an important role, in both allowing citizen to have their voice heard and receiving widespread support for change.
At the same time, we point out the importance of suitable funding opportunities for bottom-up initiatives to realize innovative ideas in border areas. Cohesion and cooperation in border regions is yet rather depended on funds like the European Regional Development Fund. Therefore, to ensure continuing of successful initiatives and sustainable improvements, we encourage health to be among the top priorities in the new programming period 2021-2027 both within ESIFs and direct funding (eg. Horizon Europe).
In February 2019, two bilingual citizen summits were organised by EPECS (European Patients Empowerment for Customised Solutions) in the Euregio Meuse-Rhine in order to collect the Citizen’s view on health. 120 citizens were mobilized and gave encouraging input on their view on “equity”, “participatory approaches” and “human resources in health”. The outcome of these citizen summits was used as input for the 25th RHN WHO annual conference in June, which had the goal to examine how to keep people at the centre of health and sustainable development policies.
 Recognising professional qualifications and skills
Recognising professional qualifications and skills
FOR HEALTHCARE IN CROSS-BORDER REGIONS WE CALL TO:
- ensure that all Member States respect EU rules on the recognition of professional qualifications;
- further strengthen Directive 2005/36/EU on the recognition of professional qualifications in extending the list of professions for ‘automatic recognition’;
- properly implement the European professional card;
- provide financial support for the digital conversion to allow a secure and fast communication between regulating authorities.
We call for a simple and swift way of recognising professional qualifications and skills for all professions in the healthcare sector. Under Directive 2005/36/EU there is already a modern system in place to regulate the recognition of professional qualifications across the EU. There are professions where automatic recognition is possible, such as for nurses, doctors, pharmacists, midwifes or architects.
Another extensive list of professions can be recognized in other EU Member States but need further application. For five professions (i. e. general care nurses, physiotherapists, pharmacists), the European professional card (EPC) was introduced in 2016 to digitally and directly communicate with the relevant regulating authorities in a secure way.
Nevertheless, this progressive Directive 2013/55/EU has not been fully implemented by most Member States (In March 2019, the European Commission took further steps in infringement procedures against 26 Member States to ensure implementation of EU rules on the recognition of professional qualifications). We encourage the Commission and MS to fully implement this directive, to look at the non-extensive list of professions, especially with a focus on health professions, and to extend it where appropriate. A full implementation of the European professional card with related digital conversion is also desirable. Especially the profession of health assistance, a broad occupational group with varying competences, qualification, training and professional title across EU Member States, is rather unregulated and incomparable at this stage.
A simple and swift way of recognising professional qualifications and skills would pave the way for health professionals living in border regions to work across the border and simultaneously close to home. With the right approach, rural exodus can in the best case be decelerated and/or partly prevented. Moreover, the possibility for jointly used health infrastructure in border regions can be created, which would – at the present moment – have a too small pool for qualified staff available.
The Hospital de Cerdanya, jointly funded and managed by the healthcare authorities of France and Catalonia/Spain, is the only binational hospital in Europe, and it operates within EU legal framework as a “European Grouping of Territorial Cooperation”.
Since September 2014, it provides specialised and emergency healthcare to 32.000 permanent residents (three times as many during the tourist seasons). Roughly 55% of the population is on the Spanish side of the Pyrenees and 45% on the French side.
Many obstacles have been overcome since day one, with no benchmark to compare to. At the present, two major cross-border projects are underway. “When emergencies erase borders” aims to facilitate the operation of Catalan and French emergency services on each other’s country when needed. Speedy mutual recognition of professional qualifications is instrumental to the former. In both cases, EU-based legal solutions are being considered, and EU aid is being provided, via the B-Solutions initiative.
 Innovative financing and payment mechanisms
Innovative financing and payment mechanisms
FOR HEALTHCARE IN CROSS-BORDER REGIONS WE CALL TO:
- map and analyse individual financing and payment mechanisms between MS when citizens access healthcare across the border;
- find innovative solutions for financing and payment of cross-border healthcare services that can be applied in border regions (e.g. to overcome differences in salary);
- support dialogue and cooperation among health insurers.
The different organisation of national healthcare systems in Member States with diverse financing and payment mechanisms may hamper cross-border collaboration in health at first sight. The Cross-Border Healthcare Directive and the EU rules on the coordination of social security systems (Regulation (EC) No 883/2004) provide the Union’s legal framework on patients’ mobility. However, they follow different structures and principles on providing reimbursement of cross-border healthcare. Therefore, in their practical implementation at national and regional levels, certain difficulties tend to arise from a cross-border regional context. Nevertheless, already existing projects in cross-border health demonstrate that binational or even tri-national cooperation and financial coverage of health services and activities is possible in a European framework – e.g. the cross-border hospital in Cerdanya (ES-FR), under the framework of a European Grouping of Territorial Cooperation (EGTC).
Sustainability of such working pilot projects need to be ensured, either through continued financial support from EU funds or in the best case, the project solutions get embedded in the structure of health systems. At this stage, the political willingness is often given but the cooperation is nevertheless slowed down by stakeholders, who do not feel responsible for cross-border work.
In the INTERREG V-A Austria-Czech Republic project “Healthacross for future” between Lower-Austria and Czechia a study will be carried out to find applicable reimbursement solutions for cross-border healthcare. Two ideas will be examined. The first is the exchange of medical services alongside the border. It is the fundamental idea that money does not follow the performance, but that different medical services with an equal total amount of health care spending will be exchanged. The basket for health care services that can be exchanged will be limited. The second is to find innovative accounting modalities. Thereby relevant stakeholders (e.g. national health insurances, hospitals;…) will work together to set up a common catalogue to bill medical services that will be provide don the other side of the border.
Since January 2017, the “Ostbelgien Regelung” allows citizens from the German-speaking Community of Belgium to access cross-border healthcare services in hospitals, day clinics and specialist practices in German border areas. The Belgian health insurance thereby reimburses health care services with the German tariff if a certain form is previously requested. Without this regulation, patients would only receive reimbursement up to the Belgian tariffs, even if the treatment in Germany is more expensive.
 Coordination of health services and investments
Coordination of health services and investments
FOR HEALTHCARE IN CROSS-BORDER REGIONS WE CALL TO:
- introduce a detailed mapping of healthcare infrastructure in cross-border areas;
- start joint coordination of health services and investments;
- design a prototype of potential shared facilities, services and care.
In the light of using health infrastructure and high-technology devices which are situated close to the border jointly, a detailed mapping of those is worth striving for alongside internal borders. The mapping can be an important foundation for common planning, commissioning and management of health services (e.g. infrastructure, capacity) between MS and the starting point for cross-border collaboration to use synergies and complement existing realities. Information on healthcare providers in border regions could also be used by national contact points (NCPs; see next chapter) to provide potential patients with relevant information. Future planning should therefore include the “cross-border” perspective, probably on a NUTS 3 level, to include the health needs of citizen from both neighbouring countries. For this task, both political leadership and strong commitment from health stakeholder are sticking points to make a difference.
In this coordination process, we stress to recognize the trend of changing health needs of citizens and how healthcare is delivered. Since cross-border collaboration in healthcare is seen rather new, it can easily comprise innovation in healthcare models. We therefore want to underline again the importance of participatory approaches for developments at regional level in the healthcare sector. Citizens in their roles as insured persons, carers, border residents and patients must play a central role in this process. They need to be at the heart of transformation process and should be included in the dialogue and cooperation to rebuild trust in the system.
In May 2019, the first cut of the spade was made in the city of Gmünd between Lower Austria (AT) and South Bohemia (CZ) for an outpatient treatment centre, that in the future will be accessible for both Austrian and Czechian patients to receive ambulatory treatments. Since doctors will be contracted, health services will be covered by social health insurances from both countries.
 Strengthening National Contact Points
Strengthening National Contact Points
FOR HEALTHCARE IN CROSS-BORDER REGIONS WE CALL TO:
- set initiatives to build trust in National Contact Points (NCPs);
- strengthen the awareness of NCPs;
- define a supportive role for NCPs and support MS in properly establishing them;
- anchoring NCP regionally.
To ensure that information on patients’ rights in cross-border healthcare are available for patients, the Directive 2011/24/EU on the application of patients’ rights in cross-border healthcare includes regulations on how to establish national contact points in Member States. NCPs are national institutions, which are operated and financed under the responsibility of each Member States. They are set up with the purpose of facilitating the provision of information on patient’s rights and entitlements, healthcare providers, complaints procedures and legal and administrative options available to settle disputes to mobile patients (Article 6 (5)). Following the Directive 2011/24/EU, national contact points shall moreover closely cooperate with each other (Article 6 (2)), consult with patient organisations, healthcare providers and healthcare insurers and there is the possibility for MS to establish “one or more” (Article 6 (1)).
We would like to see national contact points in a more supportive role for citizens, health care providers and patient organisations. The function of NCPs is often not well known by citizens and they lack awareness. The physical distance between the often nationally established NCPs and patients in border regions might also be a bit too great to allow a sense of responsibility. Anchoring national contact points regionally or ensuring regional contact persons could help to overcome this distance. Moreover, differences in governance and financing of the NCPs persist across Europe resulting in a considerable variation of services provided to EU citizens.
 Support ECBM
Support ECBM
(European Cross-Border Mechanism)
FOR HEALTHCARE IN CROSS-BORDER REGIONS WE CALL TO:
- support the adoption of the ECBM on EU level.
With great interest we follow the European Commission proposal of a regulation on a mechanism to resolve legal and administrative obstacles in a cross-border context, published on the 29th of May 2018, as part of a package of four legislative proposals establishing the framework for EU cohesion policy post 2020. The mechanism would enable a joint project to be implemented and governed by a single set of rules. The Member State where the project is located could incorporate in its legal order the rule of the neighbouring Member State. Such mechanism would simplify cross-border collaboration enormously, overcome problems related different legal frameworks and allow border regions to take full advantage of their economic, social and territorial potential.
 Data Management
Data Management
FOR HEALTHCARE IN CROSS-BORDER REGIONS WE CALL TO:
- support MS in their efforts to acquire or make existing health data accessiblein order to show health trends in regions for policy planning;
- share good practices on interoperabilityfor smooth and secure sharing of data;
- acquire health data to show health trends in regions for policy planning;
- support the shift towards Value-Based healthcare.
Data collection and sharing can show necessity and savings of cross-border collaboration. There is a clear need to have access to different regional data and to develop comparable indicators (eg. Overweight, life expectancy, smoking, alcohol consumption, medication abuse, patient mobility).
Development of eHealth strategies at EU, National and regional level is needed to ensure interoperability. While the uptake of digital technologies is growing rapidly, the deployment of interoperable digital solutions across Europe is slow. The risk is a fragmented scenario, which, especially in border areas would undermine on the long-term the (eu-)regional cooperation. While ensuring that EU citizens have secured access to their data, the European Commission needs to support Member States and regions in the development and implementation measures to monitor the cross-border interoperability of European Health Record systems.
Acquire health data is crucial to show health trends in regions for policy planning. Both the European and regional dimension of data should be taken into consideration when developing cross–sectoral policies (eg. health, environmental and social policies) in Europe. The development of a European regional database could help this exercise. Moreover, the information gathered could support, for instance, the policy development within the framework of the European territorial cooperation, eg. INTERREG programmes, thus responding to pre-conditionality requirements of ESIF.
Digital health and data management should also support the shift towards VBHC through IT platforms with six essential elements:
- Patient-centeredness;
- Use of common data definition;
- Encompass all types of patient data;
- Medical record accessible to all parties involved;
- Templates and expert systems for each medical condition;
- System architecture easy to extract information.
In the Euregio Meuse-Rhine, the project “Towards cross-border health data for the EMR” was started in 2017 by euPrevent and GGD Zuid Limburg. Together with German and Belgian partners they are establishing a long-term collaboration to collect, analyse and compare existing data and make these data available on a (EU) regional level. The commitment of the partners and data suppliers is important to overcome hindering factors like the use of different definitions, different reference dates and the frequency of health surveys.
Furthermore, the euregional partners are collecting new data in several Euregional projects. Examples are the Youth Euregional Scan (YES) and the Social Norms Approach (SNA) and Senior Friendly Community (SFC) projects. All comparable data will be presented in an online tool that will be available from November 2019 onwards: the Euregional Health Atlas. The Euregional Health Atlas will meet the wish to compare the health status in the EMR and provides insights in similarities, differences and opportunities for policy making.
Conclusion
With this joint statement, we want to emphasize the opportunities of cross-border cooperation in healthcare and encourage all stakeholders to take further action to ensure equitable access to quality healthcare for all.
Endorse the Joint statement
 The Joint statement was drafted by Healthacross Initiative and EUREGHA (European Regional and Local Health Authorities network) in partnership with various stakeholders in the framework of the 2019 Thematic Network on Healthcare in Cross-border regions on the EU Health Policy Platform of the European Commission and is open to further endorsements.
The Joint statement was drafted by Healthacross Initiative and EUREGHA (European Regional and Local Health Authorities network) in partnership with various stakeholders in the framework of the 2019 Thematic Network on Healthcare in Cross-border regions on the EU Health Policy Platform of the European Commission and is open to further endorsements.
The primary purpose of the treatment of your data is to add you on the list of endorsers. To this end, we will use your Name and Surname if you are an elected official, or the logo of the organisation you represent.
Secondarily, and only if you opt in to receive updates on the Joint Statement campaign, we will insert your data (e-mail address) in a database to keep you informed.
In both cases the EUREGHA Secretariat will treat your data for the only purpose(s) mentioned here.
The Secretariat is based in Rond-Point Robert Schuman 11, 1040 Bruxelles – Belgium. You may contact it writing to secretariat@euregha.net
Endorsers
Individuals
Biljana Borzan, Member of the European Parliament, ENVI Committee
Tomislav Sokol, Member of the European Parliament, ENVI Committee
Find an overview of all the endorsers here.